Antibiotics represent some of the most commonly taken medicines worldwide. They are a class of drugs that have been directly responsible for saving millions upon millions of lives since their discovery. Yet, there are still a lot of unknowns regarding antibiotics, their past, and their future use, however. With growing concerns over the misuse of antibiotics and the scary prospect of antibiotic-resistant “superbugs,” many questions have arisen about how best to approach the taking of antibiotics. It was the topic of conversation as Dr. Ray Woosley, founder of Crediblemeds and the Critical Path Institute chatted with KVOI’s Bill Buckmaster on his monthly “Your Meds” segment.

Antibiotics are largely thought to have been “invented” in one way or another during the early 20th century. In fact, antibiotics have occurred naturally on earth for eons. Think of it as a “constant war” between microorganisms trying to get a leg up on each other as years passed in a fight for survival. Bugs have developed ways to kill other bugs for as long as we can tell. Needless to say, we’re latecomers when it comes to cultivating our own antibiotics. When it comes to antibiotic resistance, it’s also has already been going on! The real problem is that the way we are using our newer antibiotics is having a large effect on how quickly that resistance is developing.
Prior to the widespread use of antibiotics, some of the most common medical conditions could be fatal for otherwise healthy individuals. Some of these common conditions include ear and tonsil infections, and postpartum infections in women. It’s important to remember that although these medicines have saved millions of people over the years, we need to use these medicines safely and intelligently. Bacterial resistance to the most common antibiotics is inevitable, and the medical community needs to be prepared for when that eventually occurs by having replacements lined up and ready.
Rapid resistance comes about largely due to the overuse of antibiotics, which is more often unintentional. Many times, a patient will be prescribed an antibiotic for a viral infection or just an allergy, when they should instead be given a completely different treatment or none at all. Therefore, it is critical to be certain that patients are only being prescribed antibiotics for bacterial infections that are likely to be responsive.
Patients should not be disappointed when their doctor chooses not to recommend an antibiotic. The vast majority of upper respiratory infections are in fact viral, and therefore not responsie to antibiotics. The bottom line is, don’t try to force your doctor into prescribing antibiotics if they have reservations. And always remember, if you develop any adverse symptoms after taking antibiotics such as a rash, itching, or palpitations, immediately cease treatment and consult your doctor.
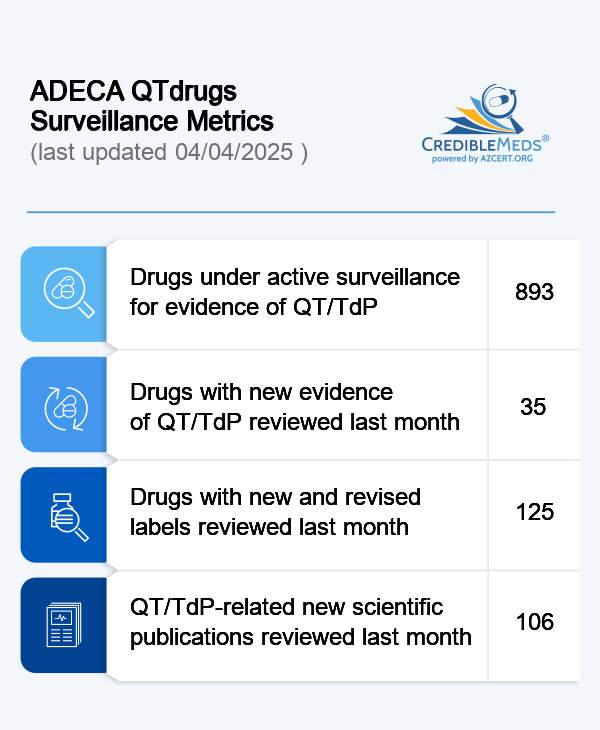
Stay safe when using antibiotics or any other medications. Consult the CredibleMeds drugs list online or through our mobile app to be a more informed patient when it comes to the medicines you take daily.
Interested readers can listen to this archived broadcast by following the link below. The “Your Meds” segment begins at 44:35.
http://www.buckmastershow.com/shows/2016/12-6-16.mp3